LOng COvid Multidisciplinary consortium Optimising Treatments and servIces (LOCOMOTION) National Research Study
The LOCOMOTION study is funded by the National Institute of Health and Care Research (NIHR) as part of a £20 million call to fund research into Long COVID (LC) in 2021. There are an estimated 1.9 million people in the UK (2.9% of the population) experiencing self-reported LC (as of 5 March 2023, data from ONS). Its aim is to use the developing science around LC to guide how health services manage the condition and ensure that patient views and outcomes are at the heart of LC services.
Chief Investigators of the project are Prof Manoj Sivan (University of Leeds) and Prof Brendan Delaney (Imperial College London)
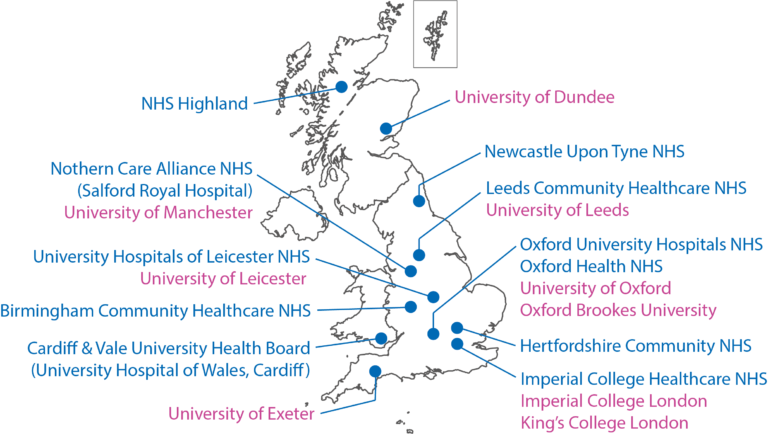
The study team is formed of eight university partners and ten NHS clinical sites (LC services) participating in the study.
The research is divided into three workstreams:
Workstream 1
Led by the University of Oxford (Prof Trish Greenhalgh), workstream 1 is exploring the evidence behind what clinics and GPs should do in terms of investigation and treatment. We recognise that the ‘root cause(s)’ of LC are not yet known, but there is still much that can be done to improve functioning, ability to work, and quality of life. We are currently producing a series of reviews and practice guides as scientific publications. We will consult with patients on the new guidelines for care, which we will implement and study in the participating LC services. The workstream is also exploring the inequalities in provision of LC care and producing specific guidance for vocational rehabilitation (return to work).
Workstream 2
Led by the University of Leeds (Dr Manoj Sivan), workstream 2 is monitoring outcomes (symptoms and responses to therapy) monthly to determine how the clinic activities affect patients and their symptom fluctuations. This is achieved via completion of the C19-YRS symptom questionnaire, which was developed in Leeds and has been adopted by the World Health Organization. The questionnaire has been rolled out in all ten participating LC services via a digital app (ELAROS), with online and paper alternatives available. In addition, we are using Fitbits and other sensors in a group of up to 400 patients to dig deeper into understanding of fatigue and the triggers for it. We aim to try and predict the kind of activities that make symptoms worse and use this data to aid self-management of LC.
Workstream 3
Led by Imperial College London (Prof Brendan Delaney), workstream 3 is working with data from the health system (LC services and GPs) to provide numerical answers to questions of how effective different LC services are. We can make comparisons between LC services as they have slightly different operating models (staff specialisms, remote vs in person, etc.). This means we can observe the differences in care provision as an onlooker without intervening. We are using retrospective data from patients seen in LC services over the past two years, and GP data via North-West London Whole Systems Integrated Care, alongside national data from the Royal College of GPs Research and Surveillance Network (with approval from the Health Research Authority).
We are also working to develop an economic model that will help the NHS determine the most effective and efficient ways of healthcare delivery. University of Oxford is delivering Work Package 3.2 utilising health economic data collected via ELAROS who are supporting this additional work package through its C19-YRS digital application
ELAROS' role
ELAROS’ digital platform was implemented in the 10 participating research sites following approval by local information governance teams to assure its safety and conformity with the necessary data management and clinical safety standards to put in patients’ hands.
All participating research sites were also offered to use the platform for routine clinical practice to run alongside research. The digital system supported this dual-use by incorporating bespoke functionality to gather the necessary consent from patients who wish to participate in research, electronically rather than on paper, to help streamline the onboarding process, reduce staff time / cost, and increase the recruitment rate for the study.
By gathering explicit consent from patients for these defined purposes, ELAROS’ system is able to automatically pseudonymise (anonymise data and link records over time) patient data and segregate research participants who have given consent to sharing their data from non-consenting patient participants. This data can then be filtered and shared with the authorised research organisations for the relevant work packages – University of Leeds (WP2.2) and University of Oxford (WP3.2).
Outputs
An up-to-date list of outputs from the study can be found here.
They are mainly intended for a more scientific audience and consist of:
- Scientific Publications. – Scientific articles that have been produced to share results and knowledge derived from the study.
- Pre-Prints. – Scientific articles that have not yet been peer reviewed.
- Lay Summaries. – A way of communicating scientific publications in ‘plain language’.
- Scientific Presentations. – Presentations, talks, and posters, exhibited at events such as national conferences, to communicate our study findings.
![]()
The outputs listed focus specifically on those generated as part of the LOCOMOTION project. However, our investigators have wide-ranging interests in Long COVID and their other relevant publications are highlighted in our News section. You may also like to look at our team members’ personal web pages which will highlight their other scientific publications. Additionally, resources specifically for patients are listed in our ‘For patients’ section.
NHS England's National Service Evaluation
Recognising the widespread uptake of ELAROS’ platform across the NHS in England, in great part due to LOCOMOTION which facilitated its implementation in 6 new English sites, NHS England commissioned University of Leeds in 2023 to undertake a national service evaluation of NHS Long Covid services using data collected via ELAROS from patients that provided consent to sharing their data for these purposes. An additional 8 clinical sites already using ELAROS for routine clinical care joined the service evaluation following approval from local IG and R&I teams.
The aims of the service evaluation were to understand a) the extent of symptom burden and functional disability in individuals accessing care in NHS-funded LC services; and b) condition trajectories and the extent of change in the severity of the condition in individuals receiving care in these services. This report provides details on data collection methods, participants, PROM data analysis, interpretation of results, and clinical implications. The report also describes the limitations in interpreting the results and makes recommendations for future work to be undertaken by NHS England, LC services, local commissioners, and individuals with LC.
National service evaluation outcomes:
Patient characteristics: A sample of 5,318 patients from 14 participating NHS LC sites were analysed. The sample had a female: male ratio of 2.1:1. The average age was 48.4 yrs, with 87% (of those whose ethnicity was recorded) of white ethnicity and 9% of Black or Asian ethnicity.
Comorbidities: This sample of patients had a low prevalence of co-morbidities (7%) with a clear onset of new LC symptoms after their COVID-19 infection supporting the onset of a new condition in previously healthy individuals.
Duration of LC: The average duration of LC in this sample was 384 days (>12 months) at first assessment in an LC site, with symptoms still ongoing at presentation, with more than 90% of the sample being non-hospitalised patients.
Digital platform: A total of 17,471 PROMs (C19-YRS and EQ-5D-5L) were completed by this sample of patients with at least 1,532 participants completing multiple assessments on the same PROM on the ELAROS digital platform.
New-onset disability: 3,395 patients who completed at least one C19-YRS questionnaire at first assessment showed significant new-onset symptom burden, functional disability and deterioration of overall health since the COVID-19 infection.
Comparison between LC and other chronic conditions: The cross-sectional EQ-5D-5L index
value of 3,438 patients suggests the burden and disability in LC are worse than that reported in the literature on Diabetes Mellitus, COPD, Heart Failure, and Multiple Sclerosis.
3-month follow-up: Among those who completed an initial C19-YRS assessment and another at 3 months, there was a statistically significant improvement in symptom burden, functional disability, and overall health. Patients at 3 months however still had significant new-onset LC symptom burden and disability compared to their pre-COVID-19 health status, i.e., their condition had improved but they were far off from complete recovery. Among those who completed EQ-5D-5L, at first assessment and at 3 months, their EQ-5D-5L index score did not show any statistically significant improvement but the EQ-5D-5L VAS showed a statistically significant improvement.
6-month follow-up: Among those who completed measures at the first assessment, 3 months, and 6 months, C19-YRS and EQ-5D-5L VAS showed statistically significant improvement whereas EQ5D Index Value showed statistically significant deterioration. Patients at 6 months however still had significant new-onset LC symptom burden and disability compared to their pre-COVID-19 health status, i.e., their condition had improved but were far off from complete recovery. The follow-up changes in scores support the efficacy of interventions provided by LC sites and suggests continued specialist input is needed to manage these patients.
C19-YRS (Condition-specific measure) vs EQ5D-5L (generic measure): Both the 3-month and 6-month follow-up changes in scores highlight that C19-YRS is a more sensitive measure than EQ5D-5L in LC. This is in keeping with the literature recommending the use of condition-specific measures.
Vocational problems: 62.5% of this sample had their work role affected with them having to either be on sick leave, reduce hours, change roles, or quit roles. Only 21% were able to maintain their previous roles held prior to their COVID-19 infection. This is suggestive of considerable productivity loss and financial implications to the country.
Fluctuating condition: In patients who completed multiple assessments, it was evident that LC is a fluctuant condition with no necessary linear trend of improvement or deterioration in terms of symptom burden, functional disability, and overall health. This highlights the need to understand the triggers for the condition and invest in self-management and ongoing support from community healthcare services.
Long-term condition: In most patients in this sample, LC has clearly become a long-term condition (LTC) with fluctuations in their condition causing disability and significant deterioration of their overall health status seen even after 18 months of LC with no complete resolution or full recovery. There needs to be a national investment in managing this new LTC along with other LTCs.
Recommendations for Healthcare Authorities
• Recognise LC is a new-onset condition with a significant burden of symptoms, functional disability and decline of overall health in affected individuals. Even though there is a lack of a single uniform biomarker yet for the condition, the findings of this study support a significant healthcare burden in previously healthy and functioning individuals.
• Recognise that in many individuals, LC is an LTC with fluctuations and requires long-term care with a similar strategy as other LTCs. The funding and commissioning plan needs to have LC included under the LTCs category and prioritise LC as much as other LTCs.
• Encourage all LC services to use a digital interactive PROMs platform as they are an efficient and cost-effective way of capturing true trajectories of the condition. There is a need to address the barriers of digital exclusion and ensure adequate training facilities are available for individuals to take up the use of such technology.
• Encourage more sites to join the NHSE national service evaluation study. With more than 700,000 patients with LC > 2 years, there is a need to capture long-term outcomes on a bigger dataset of patients than this study.
• We need to ensure we don’t lose sight of the magnitude of LC and its burden on people’s lives (finding of this study). The key is to operationalise existing LC clinics as clinical research centres and facilitate as much translational research as possible to understand the condition better and improve outcomes for patients. Studies such as LOCOMOTION and other NIHR-funded studies aim to achieve this. We need more investment in clinical interventional research in this new LTC.
Recommendations for LC services
• Continue to provide specialist care to individuals with LC. Many individuals improve substantially and are successfully discharged but services have a considerable number of patients struggling with long-term symptoms and disability which require close monitoring and targeted interventions. NHSE plans to do more work on how these services will integrate/ work with other services for other long-term conditions so that the care provided is cost-effective.
• Services need to use LC condition-specific measures such as C19-YRSm or others (for e.g., Symptom Burden Questionnaire (SBQ) as LC is a novel condition and the using a combination of symptom-based measures is cumbersome and burdensome to the patients. Using C19-YRSm along with a healthcare utility measure such as EQ5D-5L provides the right balance of measuring symptom burden and disability for the patient (C19-YRSm) and cost-effectiveness of services for the service providers and commissioners (EQ5D-5L).
Recommendations for individuals with LC
• Having a clinical diagnosis is key to successful intervention and long-term management.
Individuals with persistent symptoms need to present to their clinicians and seek specialist input.
• Complete PROMs on a regular basis to understand the fluctuations in the conditions and self-manage in terms of making adjustments to triggers and dealing with complications and functional limitations seen in the condition.
• Continue to peer-support each other and work closely with healthcare professionals and healthcare providers to enhance our understanding of the condition and invest in long-term care and further research in the area.
